Vitamin B12 is an essential nutrient, and a deficiency can cause serious health problems. If you think you may have experienced a vitamin B12 misdiagnosis or a delayed diagnosis, contact one of our medical negligence solicitors

Medical negligence
Physician Associates and Anaesthetic Associates - What do they do?
Physician Associates (PA) and Anaesthetic Associates (AA) have been in the news lately, but not everyone knows what they do within the NHS. We aim to shed more light on who they are and what they do within the healthcare system.
Who are they and what do they do?
Physician associates (PAs), Anaesthetic Associates (AAs), and Surgical Care Practitioners (SCP) belong to a group of healthcare professionals called Medical Associate Professions, or MAPs. These roles have been considered by the UK government as one of the ways in which workforce pressures within the NHS could be alleviated, and it reflects the trend towards the development of multi-disciplinary teams to meet the growing demand within the health service. Information from the British Medical Association (BMA) says that as of 2021, there are around 3000 qualified PAs and 300 AAs working within the NHS.
According to NHS employers, physician associates (PAs) are healthcare professionals with a generalist healthcare education who work alongside doctors and surgeons providing medical care as an integral part of the multidisciplinary team. They work alongside other healthcare professionals as part of the multi-disciplinary, and autonomously with the right support. They are found working in both primary and secondary care settings over about 20 specialty areas like GP surgeries and emergency medicine. They work under the supervision of a senior doctor, and could do some activities such as:
- take medical histories from patients
- perform physical examinations
- seeing patients with long-term (chronic) health conditions
- develop management plans
- provide health promotion and disease prevention advice for patients
Anaesthetic associates used to be called ‘physician associates (anaesthesia) or PA (A)’ was introduced in 2004 and they are highly trained, skilled practitioners who work as part of the anaesthetic team under the direction and supervision of a Consultant Anaesthetist. AAs play a role the assessing the patients before they go for an operation (pre-operative assessment), provide sedation, help in cardiac arrest teams, and are beneficial in supporting education for colleagues and students. They can also be engaged with local research projects and audits.
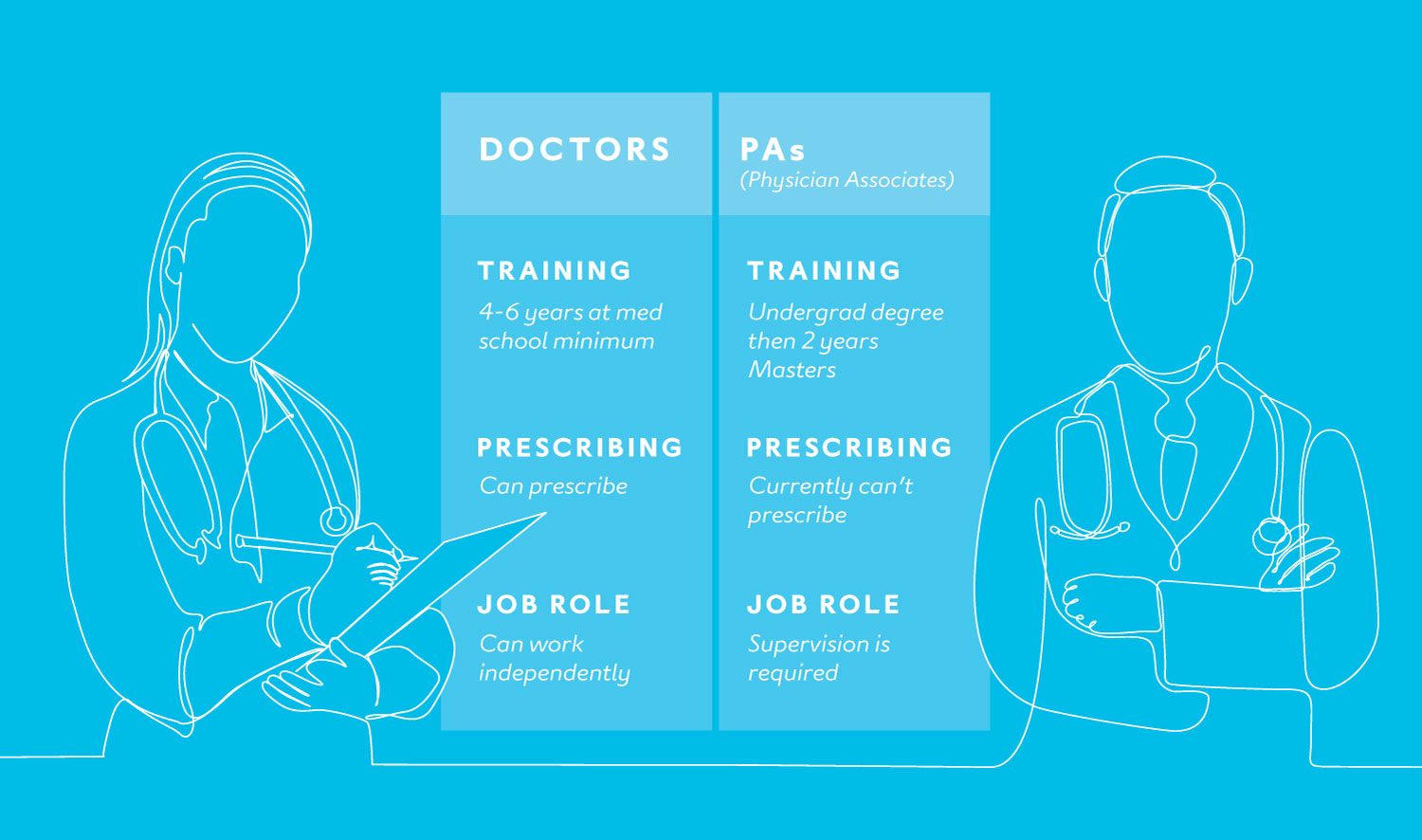
Physician Associates are trained differently to medical doctors. The below infographic illustrates the main differences between them:
PAs and AA’s are what the British Medical Association would describe as ‘direct entry roles’, whereas to be a surgical care practitioner, one already needs to be a registered healthcare professional. MAPs undergo about 2 years of Master’s level training (and relevant practice hours for clinical skills), but each have slightly different entry requirements.
SCPs are required to be a registered professionals prior to qualify for SCP training, meanwhile PAs and AAs need an undergraduate science degree to be eligible for training, although AAs can also train experienced registered healthcare professionals (nurses and physiotherapists) with at least 3 years of experience and evidence of recent academic study.
There have been increasing calls to regulate PAs and AAs and on the 26 February, the regulation entitled ‘Anaesthesia Associates and Physician Associates Order 2024 was debated in the House of Lords, and both Houses of Parliament have approved the new law, which means the regulation can be made into law. It means that once it gets implemented, PAs and AAs will go on the register of the General Medical Council (GMC), who will oversee their work, and can set conditions to ensure adequate training and fitness to practice.
The Royal College of Physicians, along with the GMC, both call for additional education, a defined scope of practice and guidance, which will hopefully be brought by regulation. The BMA has opposed the government intention for PAs and AAs to be regulated by the GMC, and said that they believe it should be another regulatory body, the Health and Care Professions Council (HCPC) that should regulate them. They also set out a guide setting out how MAPs should work safely.
The BMA also raised concerns that the new law allowing the GMC to regulate PAs could “confuse doctor and PA roles and risk patient safety”. In their website, the BMA called for a halt in the recruitment of PAs and AAs and calls on the government to regulate MAPs separately from doctors, or if the GMC regulates MAPs, demand for a separate register.
Why regulate PA’s?
PAs who have passed their Physician Associate MSc are currently placed on what is called a Physician Associate Managed Voluntary Register once fully qualified and approved. This register is held by the Royal College of Physicians and they “strongly encourage employers of PAs to check the PAMVR status of the PA at regular intervals during the year”. This voluntary register was established in 2010 to provide public safety, to set standards for their education and development, and to advance towards statutory regulation.
There are several advantages to a profession being regulated. The Professional Standards Authority for Health and Social Care gave one overarching reason for regulation: to protect the public.
Being regulated means the following are met:
- standards of competence and conduct are set out which its professionals must meet to register and practice
- the quality of education and training are checked more rigorously to make sure that students who will eventually apply for registration are competent and safe to practise
- regulators are mandated to keep an up-to-date register (or list) of people that are fit to practise that profession, and people who are in the register are mandated to provide and maintain evidence that they are competent to continue working in that field
- regulators are mandated to investigate complaints about professionals under their register and decide whether they can be allowed to continue to practice, impose sanctions and conditions, or in extremely dangerous or negligent practice – get them struck off
Nurses for example, are regulated by the Nursing and Midwifery Council (NMC), and solicitors are regulated by the Solicitors Regulation Authority. All these measures provide members of the public that assurance that the professional that handles their care or concern is under strict rules to comply with best available practice and conduct in their respective fields.
How in-house medical experts support your medical negligence claim
Our in-house medical experts play a critical role in medical negligence cases. Here, Litigation Midwife, Kim Burns and Litigation Nurse, Matthew Brown explain their roles and how their medical experience translates to medical negligence claims.



It can seem daunting to advocate for yourself in healthcare, particularly if a medical professional attempts to dismiss your concerns. In this guide, we explore how you can practice self-advocacy, provide important resources, and information on where to turn if you need support.

Making a claim for medical negligence can be complicated, and the process daunting. We’ve put together a claims guide to take you through each step, and answer some of the most frequent questions we are asked.